What is Uterus Prolapse?
Uterus Prolapse, technically known as Utero-Vaginal Prolapse but also called uterine prolapse, is descent of the uterus and vagina from their normal position in the pelvis. Commonly, it results in patients who have developed vaginal defects as a result of child birth (vaginal delivery), menopause, aging and other existing factors.
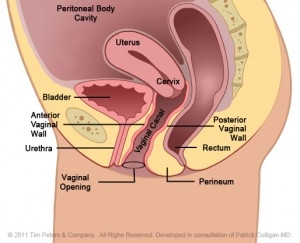
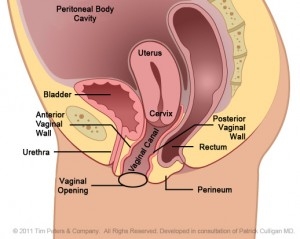
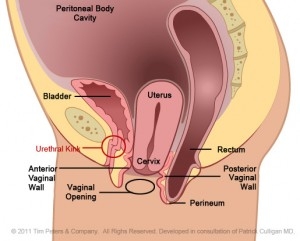
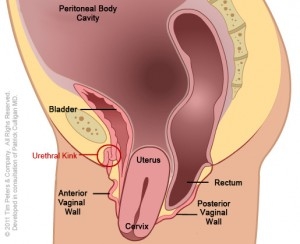
These images show the progression of advancing uterine prolapse.
Original Images Courtesy of BARD Medical – Subject to Copyrights. Labeling Enhanced for Educational Purposes by D. K. Veronikis, MD
The image on the left reflects the normal positioning of the uterus and vaginal canal within the pelvis. Moving from left to right, the image on the far right shows an advanced state of uterine prolapse. Additionally, there is weakening of the vaginal tissues in front of the cervix/uterus as well as around the uterus which allows the cervix/uterus to fall into the vaginal canal and through the vaginal opening. Also note, that this prolapse (dropping) has impacted the bladder and the rectum. Complete reconstruction of utero-vaginal prolapse must include repair and elevation of the top of the vagina, by either supporting and/or removing the uterus. Additionally, repair must include support to the remaining pelvic floor organs; the vaginal walls, bladder, rectum, and perineal muscles.
Symptoms of a Prolapsed Uterus
Women with uterus prolapse (or utero-vaginal prolapse) present with a myriad of symptoms that can reflect a bulge in vaginal compartment which may also include incomplete bladder and bowel emptying as well as urinary dysfunction, to painful intercourse. Some report difficulty in retaining a tampon; this occurs because the cervix and uterus literally descend and push the tampon down the vaginal canal and out the vaginal opening. When prolapse becomes very severe and the cervix protrudes through the vaginal opening; patients can experience bleeding from erosion of the cervix and the vaginal walls.
Treatment for Uterine Prolapse
The surgical approach utilized when treating utero-vaginal prolapse depends on the degree of prolapse, desire for fertility, and patient preference. Vaginal hysterectomy is the least invasive of all modalities with no incisions on the abdomen whatsoever. Scientific studies that are supported by several national organizations show that vaginal hysterectomy (when indicated) is the preferred approach to treating benign disease, such as prolapse. It has been shown repeatedly to have the lowest complication rate with the quickest return to normal activities.
Some patients who wish to preserve fertility, yet their quality of life is significantly altered by prolapse, may be candidates for uterine preseravtion. In these select patients, a uterine preservation surgery may be beneficial. This approach allows for future child bearing during a reconstructive procedure that will also correct the vaginal wall laxity and relaxation of the pelvic floor.