What is Vaginal Prolapse?
Vaginal prolapse, technically known as vaginal vault prolapse, and occurs in women after hysterectomy where the vaginal cuff or apex (top of the vagina-where the cervix used to be) descends down and into the vaginal canal. This condition is often mistaken as a “dropped bladder” because the patient notices a bulge in the vagina. Repairing the top of the vagina is critical to comprehensive vaginal reconstruction and successful long-term outcomes. This can and should be done at the time of hysterectomy as well as many years later as part of other reconstructive surgery.
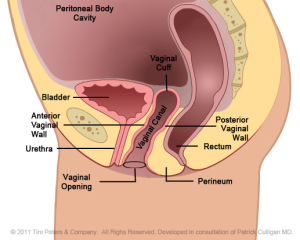
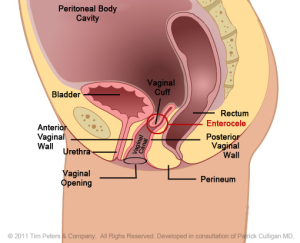
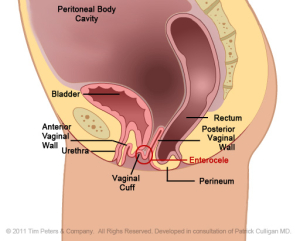
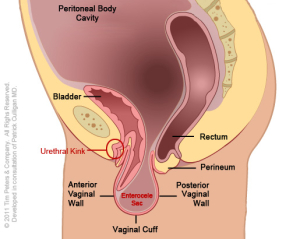
The images below show the advancing decline in the vaginal canal thus creating vaginal prolapse.
Original Images Courtesy of BARD Medical – Subject to Copyrights. Labeling Enhanced for Educational Purposes by D. K. Veronikis, MD
The image on the left reflects the normal positioning of the vaginal cuff in the pelvic floor after a hysterectomy. Moving from left to right, the image on the far right shows an extreme case of vaginal vault prolapse. Additionally, there is weakening of the vaginal tissues supporting the anterior vaginal wall. This pressure, in the advanced case, from the prolapse creates a “kink”, an obstruction, with the urethra which leads to difficulty with bladder evacuation. Additionally, there is weakening of the vaginal tissues supporting the posterior vaginal wall. In an advanced case, this pressure creates a “pouch” in the bowel wall. This obstruction can lead to difficulty with bowel evacuation.
Furthermore, the weakening of the vaginal cuff, as well as the anterior and posterior vaginal wall supportive structures, has permitted the development of an enterocele – a peritoneal cavity hernia into the pelvis. This type of hernia defect will eventually with peritoneal pressure push the small and sometimes large bowel into this peritoneal pouch which can be seen in the advanced case. The stretch on the bowel and mesentery will create a back ache that responds to rest and laying down.
Complete and proper repair of this specific prolapse condition must include fixing the vaginal apex (the cuff), the enterocele, as well as the caliber to the vaginal canal and repairing the support to the remaining pelvic floor organs; the bladder, urethra, rectum and perineum. Singular pelvic floor defects are a rare occurrence.
Treatment of Vaginal Prolapse
Vaginal prolapse can be repaired by three surgical approaches – vaginal, laparoscopic and abdominal. The least invasive and most cost-effective of these is the vaginal approach, and this is the modality utilized for the majority of our patients presenting with a post-hysterectomy vaginal vault prolapse. Completing the repair vaginally allows for the repair of the other vaginal defects along with treating urinary and/or fecal incontinence at the same surgical site. Uncommonly, a patient will require an abdominal approach – often secondary to a shortened vagina from prior surgeries. The other patients may have had prior surgery elsewhere for vault prolapse which was unsuccessful, and to provide these patients the best result following previous attempts, an abdominal approach may be necessary.
As stated previously the most critical component of comprehensive reconstructive vaginal surgery to treat prolapse is elevation, fixation, and repair of the vaginal apex. The critical point on the vaginal cuff that becomes fixated is referred to as the apex. Whether a vault prolapse is repaired vaginally, laproscopically, or abdominally, the exact site that is chosen to be the apex is of paramount importance. If it is too close to the anterior side, it will eventually show a weakening of the posterior vagina and vice versa. Dr. Veronikis has dedicated his practice to prolapse repair and therefore; he performs hundreds of these procedures each year. Dr. Veronikis has developed a system of retraction that he utilizees to achieve a high success rate with low complications utilizing the vaginal approach. His attention to the details of repairing all of the vaginal defects also is integral to his high success of outcomes. Rarely does a prolapse of the apex exist alone, just as a cyctocele is rarely the only defect. Therefore, the key in treating prolapse is appropriate positioning of the apex and comprehensive repair to all other vaginal defects.